In the avant-garde clinics of 2077, the union of technology and healthcare will render the bustling nurses of yesteryears obsolete, replaced by a solitary AI assistant whose demeanor exudes both efficiency and warmth. With an aura of anticipation enveloping the sleek, minimalist reception area, patients find themselves in the gentle embrace of artificial intelligence, its digital gaze focused on their medical concerns.
In this cutting-edge environment, patient conversations transcend words, becoming raw data meticulously dissected by the AI assistant. Drawing upon a vast repository of electronic health records, it navigates the labyrinth of medical history with a precision that far surpasses that of a human. Each symptom and anomaly is studied with laser focus, paving the way for a collaborative endeavor between human expertise and machine intelligence.
Armed with the insights gleaned from patient data, the AI software then embarks on a journey of analysis and synthesis, uncovering hidden patterns and correlations with algorithmic finesse. In a matter of moments, it crafts a bespoke treatment plan, tailored to the individual's genetic predispositions, medical background, and even financial capabilities. As patients depart the clinic, prescription in hand, they are left to ponder the evolving landscape of healthcare, where the roles of man and machine intersect in a dance of healing and possibility.
Sounds like something out of a sci-fi movie. Well, that’s where we are headed and where we’ll end up. It is now, in 2024, that we see artificial intelligence growing into a commercial and industrial powerhouse reshaping businesses and occupations. What will it do to medical professionals?
Well, let us find out!
Brief Overview of the Rise of AI in Healthcare
Artificial Intelligence in healthcare refers to the use of advanced algorithms and machine learning tools to analyze complex medical data, make clinical predictions, and support decision-making processes in the diagnosis, treatment, and management of diseases. AI leverages large datasets, including electronic health records, medical imaging, genetic information, and real-time patient data, to generate insights, identify patterns, and optimize patient care.
Healthcare organizations, research institutions, and technology companies are increasingly investing in AI-driven solutions to improve patient outcomes, streamline healthcare delivery, and reduce costs. While challenges such as data privacy, regulatory compliance, and ethical considerations remain, the widespread adoption of AI in healthcare holds immense promise for revolutionizing the way medical care is delivered and experienced.
Human Empathy and Compassion
Empathy and emotional connection stand as cornerstones in the practice of medicine, integral to fostering trust, comfort, and ultimately, patient well-being. Medical professionals possess a unique capacity to understand and resonate with the emotions of their patients, offering not only medical expertise but also a compassionate presence that transcends the boundaries of diagnosis and treatment. This empathetic connection plays a pivotal role in the healing process, influencing patient satisfaction, adherence to treatment plans, and overall health outcomes.
However, artificial intelligence falls short of replicating this fundamental aspect of the human brain and interaction. An artificial intelligence healthcare system can process vast amounts of medical data and generate clinical insights, but it lacks the innate ability to empathize with patients' emotions or form genuine emotional connections, which is why it cannot replace physicians. The nuanced understanding of non-verbal cues, subtle shifts in tone, and unspoken fears that human doctors effortlessly navigate remain beyond the reach of current AI technology.

Moreover, the healing journey often entails navigating complex emotional terrain, where patients grapple with fear, uncertainty, and vulnerability. In these moments, the presence of compassionate and empathetic medical professionals can serve as a source of solace and support, instilling confidence and resilience in the face of adversity. The reassurance derived from knowing that one's concerns are not merely data points but are genuinely understood and acknowledged by a caring physician can significantly impact the patient's experience and overall outcome.
Complex Decision Making
In the realm of healthcare, decision-making emerges as a nuanced art, blending scientific expertise with a deep understanding of patients’ unique circumstances, preferences, and values. Human doctors, seasoned by years of training and experience, navigate this intricate landscape with finesse, crafting tailored care plans that transcend mere diagnosis and treatment.
Indeed, the essence of medical decision-making lies in the space between certainty and ambiguity, where human doctors excel, drawing upon their expertise and intuition to navigate uncertainty with grace and precision. While artificial intelligence holds promise as a tool to augment medical decision-making, it underscores the irreplaceable role of human judgment in healthcare. As we embrace technological advancements, we must ensure that patient care remains grounded in compassion, empathy, and the warmth of the human touch.
Critical Thinking and Creativity
Critical thinking and creativity stand as pillars of the medical profession, and human endeavor in general, elevating the practice of medicine to a realm of nuanced judgment and innovative problem-solving. Human doctors, trained to analyze complex medical scenarios, sift through layers of information with discerning eyes, drawing upon their expertise to navigate uncertainties and arrive at well-informed conclusions. This ability to critically evaluate evidence, weigh alternative courses of action, and adapt strategies to unique patient contexts lies at the heart of effective medical care.
AI algorithms, in contrast, operate within predefined parameters, relying on structured data inputs and rules-based logic to generate insights and recommendations. While artificial intelligence can undoubtedly augment medical decision-making by offering clinical guidelines and analyzing large datasets, it lacks the intuitive understanding and innovative thinking that characterize human doctors' approach to care.
Patient-Doctor Relationship
The patient-doctor relationship forms the cornerstone of effective healthcare, built on a foundation of trust, empathy, and mutual respect. Human doctors, with their ability to establish meaningful connections with patients, offer more than just medical expertise. They serve as confidants, advocates, and partners in the journey towards healing. Through active listening, compassionate communication, and personalized care, the medical community forge bonds with their patients that transcend the transactional nature of medical treatment, fostering a sense of security and empowerment in those under their care.

The empathetic presence of a human doctor offers a source of comfort and reassurance to patients, particularly in times of distress or uncertainty, a dimension of care that AI is inherently unable to provide.
Ethical and Moral Judgment
Ethical and moral judgment are integral components of medical practice, guiding doctors in navigating complex moral dilemmas and upholding the highest standards of integrity and patient welfare. Human doctors imbued with a deep sense of professional ethics and moral responsibility, grapple with ethical quandaries that extend far beyond clinical considerations. From respecting patient autonomy and confidentiality to balancing beneficence with non-maleficence, doctors must weigh a myriad of ethical principles and considerations in every decision they make, ensuring that their actions align with the principles of medical ethics and the broader values of society.
Contextual Understanding
Artificial intelligence struggles to grasp the contextual understanding that human doctors effortlessly navigate. An artificial intelligence healthcare system might excel in processing structured medical data and identifying patterns, but it fails when confronted with the complexities of human life and social dynamics. Contextual factors such as socioeconomic status, cultural beliefs, and interpersonal relationships play a significant role in shaping health outcomes, yet these are inherently difficult for AI to capture and interpret accurately.
Contextual awareness lies at the heart of effective medical care, encompassing a broad spectrum of factors that shape the individual health experiences of patients. Human doctors possess a unique ability to contextualize medical information within the broader framework of a patient's life, taking into account social, cultural, economic, and environmental influences that may impact health outcomes. By understanding the intricacies of a patient's lived experience, human doctors can tailor treatment plans and interventions to address not just the symptoms of illness, but also the underlying determinants of health, fostering more holistic and patient-centered care.
Adaptability to Unique Cases
Adaptability to unique cases is a defining characteristic of human doctors that sets them apart from artificial intelligence systems. Human doctors possess a remarkable ability to assimilate a myriad of clinical data and synthesize it with their depth of knowledge, experience, and intuition to navigate complex and novel patient presentations. Whether confronted with rare diseases or atypical symptoms, human doctors demonstrate flexibility and creativity in tailoring treatment plans to address the specific needs of each patient, drawing upon a nuanced understanding of both medical science and individual patient contexts.
AI systems excel in processing vast amounts of standardized data and identifying patterns within predefined parameters, but they struggle to adapt to unique cases that deviate from established patterns. The inherent variability and unpredictability of human physiology and pathology pose significant challenges for AI algorithms, which may lack the capacity to extrapolate from limited data or recognize subtle deviations from the norm.
Emotional Intelligence
Emotional intelligence stands as a quintessential trait of human doctors. Doctors possess a profound capacity to understand and empathize with the emotions of their patients, offering not only medical expertise but also a compassionate presence that transcends the confines of diagnosis and treatment. Through genuine empathy, human doctors can promote patient’s resilience in the face of illness and adversity.

In contrast, AI lacks the inherent ability to engage in genuine human interactions or comprehend the complex spectrum of human emotions. AI algorithms cannot replicate the nuanced understanding of non-verbal cues, subtle shifts in tone, and unspoken fears that human doctors understand.
Hands-On Medical Procedures
Hands-on medical procedures represent a domain where human doctors excel, leveraging their dexterity, tactile sensitivity, and fine motor skills to perform manipulations with precision and expertise. Whether conducting surgical interventions, administering injections, or performing physical examinations, human doctors rely on their hands as invaluable instruments of healing, guided by years of training, experience, and intuition. The tactile feedback and real-time adjustments afforded by hands-on procedures enable human doctors to adapt their techniques to the specific needs of each patient, ensuring optimal outcomes and minimizing risks.
On top of that, the hands-on approach to medical procedures embodies more than just technical skill—it encompasses the human connection through physical contact, providing comfort, reassurance, and a sense of trust to patients in their time of vulnerability.
Accountability and Responsibility
Accountability and responsibility serve as foundational principles in healthcare, reflecting the ethical obligation of doctors to uphold the highest standards of care and prioritize patient well-being above all else. The average doctor carries the ultimate responsibility for their medical decisions and actions, including ethical considerations, potential errors, and consequences. AI, in turn, lacks the capacity for moral agency and accountability inherent in human judgment. Ethical considerations and the potential implications of AI-generated recommendations fall ultimately upon the human stakeholders—developers, healthcare providers, and policymakers—who design, implement, and oversee AI systems.
Where AI Will Actually Substitute People
AI holds immense potential to complement medical practice across various domains, offering valuable support in areas where it can enhance efficiency, accuracy, and accessibility. Some key areas where AI may substitute human physicians and doctors include:
- Diagnostic imaging: AI algorithms can analyze medical images such as X-rays, MRIs, and CT scans with remarkable speed and accuracy, aiding in the detection and diagnosis of diseases such as cancer, fractures, and neurological conditions. AI-powered diagnostic tests can help radiologists interpret images more efficiently, reducing turnaround times and potentially improving medical diagnostics accuracy.
- Pathology and histology: AI can analyze tissue samples and pathology slides to identify abnormalities and assist pathologists in diagnosing diseases such as cancer. AI algorithms can help streamline the process of analyzing large volumes of histological data, potentially reducing diagnostic errors and improving patient outcomes.
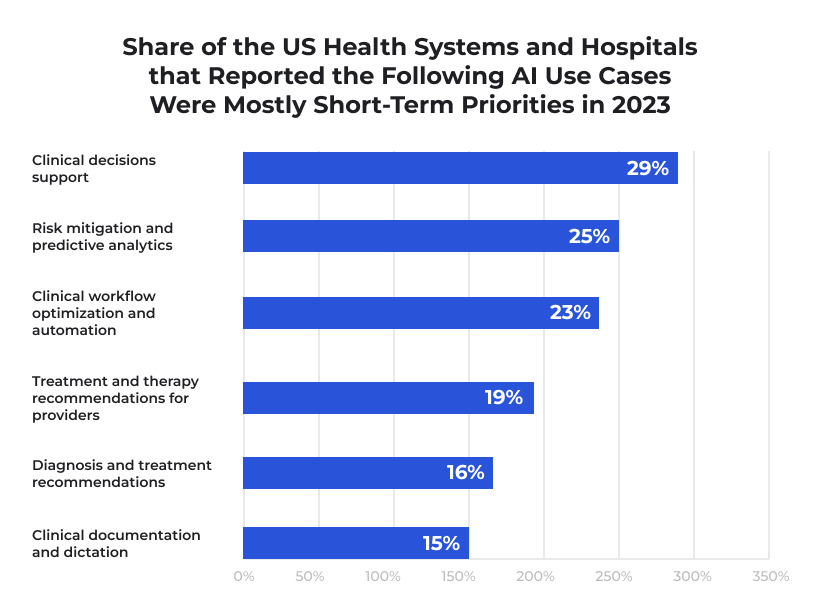
- Clinical decision support: AI-powered clinical decision support systems can analyze patient data, medical records, and clinical guidelines to provide recommendations for diagnosis, treatment, and management of various medical conditions. These systems can help health care providers make evidence-based decisions more efficiently, improving patient outcomes and reducing medical errors.
- Telemedicine and remote monitoring: AI-driven telemedicine platforms and remote monitoring devices can facilitate virtual consultations, remote patient monitoring, and personalized health interventions. These technologies enable patients to access health care services remotely, improving access to care, reducing healthcare costs, and enhancing patient convenience.
- Drug discovery and development: AI algorithms can analyze vast amounts of biomedical data, predict drug interactions, and identify potential drug candidates for various diseases. AI-driven drug discovery platforms can accelerate the drug development process, leading to the discovery of novel therapeutics and personalized treatment options for patients.

While AI has the potential to substitute certain tasks traditionally performed by human physicians and doctors, it is essential to recognize that AI is most effective when integrated into collaborative care models that leverage the unique strengths of both AI and human expertise. At the end of the day, the goal of AI in healthcare should be to enhance, rather than replace physicians, the role of human doctors, improving the quality, efficiency, and accessibility of healthcare services for patients worldwide.
Conclusion
As the rapid proliferation of AI across various sectors, particularly healthcare, becomes increasingly evident, many esteemed experts anticipate a future where AI will replace doctors and other medical professionals. AI's foundation in machine learning suggests that its impact will extend to unforeseen levels, particularly as advancements like the ability to print functional replicas of human organs become reality rather than science fiction. Healthcare, a field in dire need of innovation to combat deadly diseases and chronic injuries, stands to benefit greatly from AI's potential.
Despite the immense promise of AI-driven innovations, the prospect of AI fully replacing doctors remains uncertain, particularly given the current state of technology. Even with significant advancements, AI is unlikely to replace doctors and other medical staff members in the foreseeable future, potentially spanning centuries. Human evolution has taken hundreds of thousands of years, and it is only now that we stand on the verge of technological singularity, underscoring the complexity of predicting the future of healthcare and technology. Only time will reveal the true extent of AI's impact and the evolution of medical practice in the coming years and beyond.
So, will there still be human doctors in the clinics in 2077? Most certainly, yes, there will be human doctors making the most critical decisions, doing surgeries, and encouraging patients to keep on going.



