Remote Patient Monitoring (RPM) has moved far beyond its early experimental phase. What began as simple data collection from wearable devices has evolved into a critical digital infrastructure layer for modern healthcare. In 2026, RPM platforms are no longer side projects, innovation pilots, or “nice-to-have” features. They sit at the heart of chronic care management, hospital-at-home programs, post-operative recovery, elderly care, and preventive medicine.
This rapid evolution has fundamentally changed the nature of the challenges teams face. While clinical adoption and regulatory compliance remain important, the biggest obstacles to successful RPM deployment today are technical. Engineering decisions now directly influence clinical outcomes, operational efficiency, and economic viability.
Building a reliable, scalable RPM platform in 2026 means solving problems that look far more like real-time fintech or industrial IoT systems than traditional healthcare software. Device interoperability, signal reliability, real-time data processing, AI governance, security, and clinical workflow integration are no longer secondary concerns. They are the core of the product.
This article explores the most critical technical challenges shaping RPM platforms in 2026 and explains how engineering teams are addressing them in practice.
Why RPM Has Reached a Technical Tipping Point?
Several long-term trends have converged to push RPM into mainstream clinical use. Aging populations, rising chronic disease prevalence, persistent healthcare staff shortages, and the rapid expansion of hospital-at-home models have fundamentally reshaped care delivery. At the same time, advances in sensor technology, cloud computing, and AI have made continuous patient monitoring both technically feasible and economically viable.
As a result, RPM systems now operate at a scale that was unimaginable just a few years ago. Tens of thousands of patients may be monitored simultaneously, generating continuous streams of biometric data that must be ingested, analyzed, and translated into clinical decisions in near real time.
This scale changes everything. Systems that worked well for hundreds of patients begin to collapse under thousands. Architectures designed for batch processing fail under continuous streaming workloads. Security models built for clinical portals struggle when applied to millions of IoT endpoints. And data pipelines optimized for reporting fall apart when tasked with supporting real-time clinical interventions.
In 2026, RPM platforms are no longer judged by feature sets alone. They are judged by reliability, latency, scalability, and clinical trust — all of which are fundamentally engineering problems.
The Growing Complexity of Modern RPM Systems
To understand why technical challenges have become so dominant, it helps to look at what a modern RPM system actually consists of.
At the edge of the system are dozens of medical and quasi-medical devices: ECG patches, pulse oximeters, blood pressure monitors, glucose sensors, smart inhalers, digital stethoscopes, and activity trackers. These devices communicate via Bluetooth, Wi-Fi, cellular, or low-power wide-area networks, often using proprietary protocols.
This raw data is typically collected by mobile apps or home gateway devices, which perform basic preprocessing before forwarding it to cloud platforms. Once in the cloud, the data flows through ingestion pipelines, streaming engines, AI models, and clinical rule systems. Finally, it appears inside clinician dashboards, EHR systems, and care coordination platforms, where it influences real clinical decisions.
Each of these layers introduces technical complexity, and small architectural mistakes at any point can cascade into major system failures. As RPM scales, this complexity compounds rapidly.
Challenge #1: Device Interoperability and Fragmented Ecosystems
One of the most persistent technical challenges in RPM is device interoperability. The market is flooded with hardware vendors, each offering unique sensors, proprietary SDKs, and custom communication protocols. Even when vendors claim to follow industry standards, real-world implementations vary widely, forcing engineering teams to build custom integrations for nearly every device.
This fragmentation creates a massive engineering burden. Each new device requires weeks of development, testing, validation, and maintenance. Firmware updates routinely break integrations. Data formats differ subtly but critically, leading to normalization errors that can affect clinical interpretation.
Over time, these integrations accumulate into a fragile web of dependencies that becomes increasingly difficult to manage. Platform upgrades slow down. New partnerships take longer to launch. Technical debt grows faster than engineering capacity.
The most effective solution to this problem is architectural rather than tactical. Instead of directly integrating devices into core systems, leading RPM platforms introduce a dedicated device abstraction layer. This middleware acts as a translation engine, converting all incoming device data into a unified internal format. It isolates vendor-specific complexity from the rest of the platform and allows new devices to be onboarded without touching clinical or analytics pipelines.
When combined with rigorous use of healthcare data standards such as FHIR and IEEE 11073, this approach dramatically reduces integration friction. More importantly, it future-proofs the platform against inevitable device churn, allowing teams to swap vendors without destabilizing core systems.
Challenge #2: Data Accuracy, Signal Noise, and Clinical Trust
Data quality is the foundation of any RPM system, yet it remains one of the most underestimated challenges. While modern wearables are remarkably sophisticated, they are still subject to motion artifacts, poor placement, environmental interference, and individual physiological variation.
In practice, this means that raw sensor data is often noisy, inconsistent, and context-dependent. A sudden heart rate spike might indicate arrhythmia, physical exertion, emotional stress, or simply poor sensor contact. Without proper filtering and interpretation, RPM systems generate excessive false alarms.
Over time, this leads to alert fatigue among clinicians. When every shift produces dozens of questionable alerts, medical staff begin to ignore notifications altogether, defeating the purpose of continuous monitoring. At that point, RPM becomes more of a liability than a clinical asset.
Solving this problem requires moving beyond simple threshold-based alerts. Leading platforms now apply multi-layered signal processing techniques that combine edge filtering, sensor fusion, and adaptive calibration. By correlating multiple data streams — for example, heart rate, movement, and oxygen saturation — systems can infer clinical context and dramatically reduce false positives.
Equally important is personalization. Rather than relying on generic population thresholds, modern RPM platforms learn individual baselines over time. This allows alerts to reflect meaningful deviations from each patient’s normal state, improving both sensitivity and specificity. The ultimate goal is to deliver fewer alerts, but with far higher clinical relevance. When clinicians begin to trust alerts again, RPM becomes a true decision-support tool rather than a digital noise generator.
Challenge #3: Real-Time Data Processing at Scale
As RPM deployments grow, they quickly encounter limitations in traditional backend architectures. Systems designed around batch processing and periodic uploads struggle when faced with continuous high-frequency data streams from thousands of patients.
In these environments, latency becomes critical. Delayed alerts can mean missed deteriorations, slower interventions, and poorer outcomes. At the same time, processing vast volumes of data in real time can overwhelm infrastructure, driving cloud costs to unsustainable levels.
Modern RPM platforms increasingly rely on event-driven architectures built around streaming technologies. Instead of pushing data into centralized databases and running periodic queries, these systems process events as they occur. Each data point becomes part of a real-time pipeline that triggers analytics, rules engines, and AI models within milliseconds.
Edge computing plays a complementary role. By performing initial filtering, aggregation, and anomaly detection closer to the patient, systems significantly reduce the volume of data transmitted to the cloud. This lowers latency, improves resilience in low-connectivity environments, and cuts infrastructure costs.
Together, these approaches enable RPM platforms to scale gracefully while maintaining the responsiveness required for clinical decision-making.
Challenge #4: Security, Privacy, and Regulatory Compliance
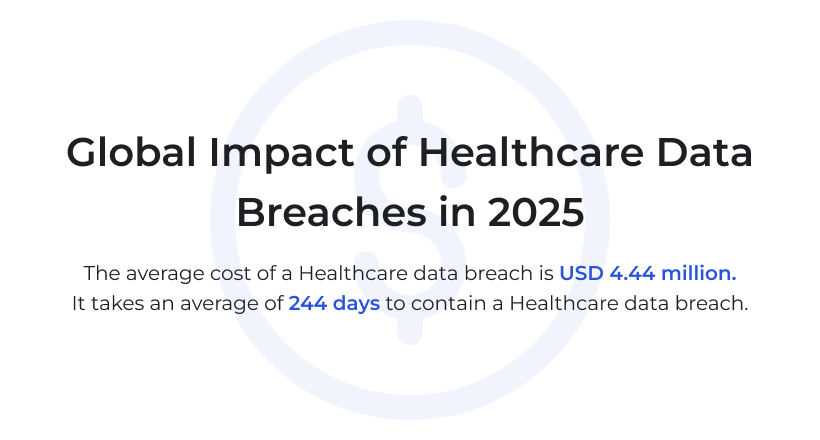
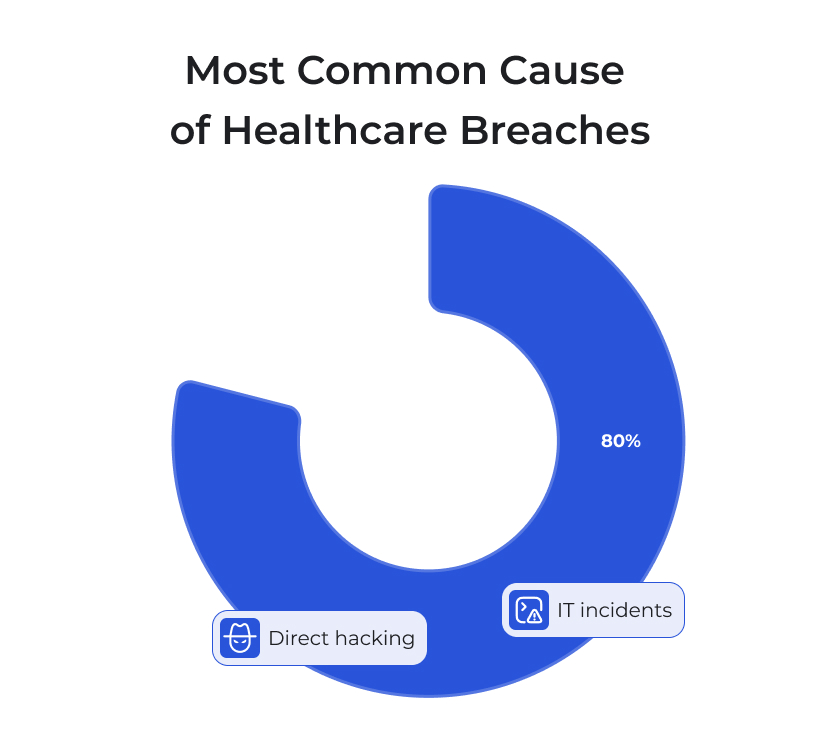
Few domains face security challenges as severe as healthcare, and RPM raises the stakes even further. Continuous monitoring systems dramatically expand the attack surface by introducing thousands of connected devices into clinical networks. Each wearable, home hub, and mobile app becomes a potential entry point for attackers.
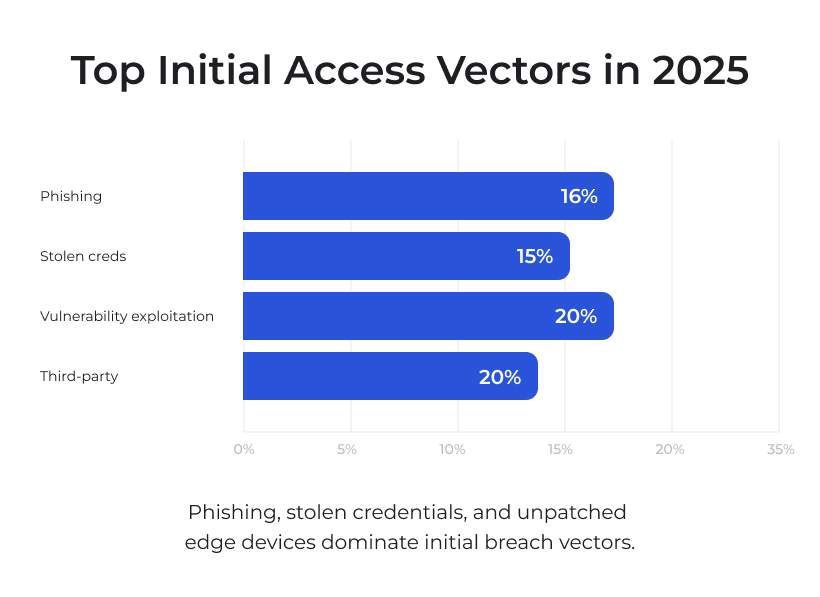
At the same time, regulatory requirements around patient data continue to tighten. Platforms must comply with frameworks such as HIPAA, GDPR, MDR, FDA software regulations, and ISO security standards. Violations can result in severe financial penalties, legal consequences, and irreparable reputational damage.
Traditional perimeter-based security models are increasingly inadequate in this context. Modern RPM systems are shifting toward zero-trust architectures, in which every device, service, and user must authenticate continuously, regardless of location. End-to-end encryption ensures that data remains protected from the moment it is generated until it is consumed by clinical systems.
Equally critical is secure firmware management. Many high-profile IoT breaches have occurred through compromised device updates. By implementing cryptographically signed firmware and secure over-the-air update pipelines, RPM platforms can prevent unauthorized modifications and ensure device integrity throughout their lifecycle.
Security in RPM is no longer a compliance checkbox. It is a foundational design principle that shapes system architecture from day one.
Challenge #5: AI Reliability, Model Drift, and Explainability
AI now plays a central role in RPM. Predictive models detect early signs of deterioration, optimize triage workflows, and support proactive interventions. However, deploying AI in clinical environments introduces its own set of technical challenges.
One of the most critical issues is model drift. As patient populations change, sensor technologies evolve, and care protocols shift, the statistical properties of incoming data gradually diverge from training datasets. Over time, model accuracy degrades, often without obvious warning signs.
This silent deterioration poses significant clinical risk. Inaccurate predictions can delay interventions or generate misleading alerts, undermining both patient safety and clinician trust.
To address this, mature RPM platforms treat AI as a continuously evolving system rather than a static component. Automated validation pipelines constantly monitor model performance, triggering retraining or rollback when accuracy thresholds are breached. Comprehensive model governance frameworks track versioning, data lineage, and clinical validation results, ensuring full auditability.
Equally important is explainability. Clinicians are understandably reluctant to act on predictions they cannot interpret. Explainable AI techniques provide human-readable insights into why specific alerts were generated, bridging the gap between complex algorithms and clinical reasoning. Without transparency, AI becomes a black box. With it, AI becomes a trusted clinical partner.
Challenge #6: Integration into Clinical Workflows
Even the most advanced RPM platform fails if it disrupts clinical workflows. Healthcare professionals operate under intense time pressure, and any additional friction quickly leads to resistance.
Many RPM systems struggle to integrate cleanly with existing EHR platforms. Differences in data standards, legacy infrastructure, and inconsistent API implementations create barriers that force clinicians to juggle multiple systems, manually reconcile data, or navigate disjointed interfaces.
The solution lies in deep, native integration. Modern RPM platforms increasingly adopt FHIR as their primary integration standard and embed functionality directly into EHR environments using SMART-on-FHIR applications. This allows clinicians to access RPM insights within their existing workflows, eliminating context switching and reducing cognitive load. When RPM becomes an invisible extension of familiar clinical tools, adoption rises naturally.
Conclusion: Engineering Is Now Clinical Strategy
In 2026, the success of Remote Patient Monitoring no longer depends primarily on clinical vision or regulatory approval. It depends on engineering excellence.
The platforms that lead the next generation of digital healthcare will be those that master real-time data engineering, resilient system architecture, AI governance, and seamless clinical integration. Technical decisions made early in product development now directly influence patient outcomes, clinician trust, and economic sustainability.
RPM is no longer just about collecting data. It is about building intelligent, reliable, and secure systems that actively shape how care is delivered. And in that transformation, engineering has become clinical strategy.



